Malnutrition Care Score for IQR
The Malnutrition Care Score quality measure is available for 2025 hospital reporting.
The Malnutrition Care Score quality measure is available for 2025 hospital reporting.
Following your completion of this section, you will know how to:
Plan for your quality improvement activities
Train team members and implement the selected clinical improvement
To formally kick-off the implementation phase, hold an “action planning” meeting with the Project Team to revisit the project goals, desired results, and expectations for sustaining those results. This initial meeting can be used to develop action plans that will serve as day-to-day guides for the project. You will also want to develop a set timeline for your project. For example, you may want to implement the change over a three-month period, with retrospective data collection for one or two months prior to implementation (to serve as your baseline) and continued data collection for one or two months following implementation to assess whether the care team is able to maintain the change.
Depending on the clinical improvement selected for the MQii, the teams should consider the feasibility of tackling multiple activities at once. It is often helpful to first focus on small, rapid cycles of change.[41] This involves first implementing one or two changes to the existing clinical workflow that align with the recommended care workflow (e.g., ensuring all admitted patients age 65+ years receive a malnutrition screening).
Once that first modification is sufficiently established in your clinical workflow, the teams can then build upon it as the care team becomes more comfortable with implementing changes to align more closely with the recommended standards of care (e.g., ensuring that once patients age 65+ years receive a malnutrition screening, as well as a malnutrition-risk diet order, a dietitian consult, and a nutrition assessment, if identified as “at risk” of malnutrition). This will allow the Care team to focus on one particular aspect of the clinical workflow at a time and more easily identify and address any barriers to effective implementation.
Additionally, implementing one or two clinical improvements at a time allows the Project Team to communicate any implementation facilitators across care teams and address any barriers that arise. While a gradual implementation approach is recommended, it is important to note that addressing all components of the recommended workflow is optimal for achieving high-quality malnutrition care.
Throughout project implementation, you should test, monitor, and evaluate changes for each phase of the clinical workflow. To do so, you may wish to follow a Plan-Do-Study-Act or similar quality improvement approach.
What are we trying to accomplish?
How will we know that a change is an improvement?
What additional changes to current practices can we make that will result in improvement?
During Step 1, if you have not already done so, you will want to select the measures/indicators you will track throughout and following implementation, as well as your targets for each of these measures/indicators following your quality improvement activity. To help achieve the targets and monitor progress on selected quality measures and/or indicators, you will need to establish:
Remember to monitor your progress and determine if sufficient improvement has been achieved before adding another improvement activity or moving on to the next phase of implementation.
In order to implement your malnutrition quality improvement activities as part of the MQii, it will be necessary to make all care teams are aware of the nutrition care focus areas selected for quality improvement. Your Project Team should also inform them of current gaps in nutrition care processes and necessary changes or modifications to the clinical workflow to better align with best practices (including where barriers exist and training on how to address them).
To provide context for implementing the MQii improvement activities, care teams should receive education on the prevalence and impact of malnutrition. To the extent that such information can be made specific to your hospital’s performance on malnutrition care (e.g., if you can pull statistics highlighting the prevalence of malnutrition in your facility and rates of readmissions or hospital length of stay in these patients compared to non- malnourished patients), the more impactful it will be.
Similarly, it is beneficial to share the MQii recommended clinical workflow and related best practices with the Care team prior to implementation so that they understand the extent of potential improvement that can be made to your existing workflow. The goal is to ensure the Care team’s knowledge attainment around the importance of evaluating patients for malnutrition, as well as best practices associated with an optimal clinical workflow.
The Project Team can then formally train the Care team on the quality improvement activities that were identified as the implementation focus for the MQii at your facility. When possible, the Care team should be trained as a group during grand rounds or lunch-and-learn sessions to allow for a greater appreciation of how individual members will work together. Adopt the approach to information sharing that best fits your organization – this may include sharing videos or PowerPoint presentations at group meetings, using pocket cards, posting flyers in break rooms, or other tools to raise awareness of malnutrition and optimal care practices. All team members should understand their role within the Care team, how data are being collected, and the quality measures and/or quality indicators that the data collection is assessing.
Below is a list of recommended training presentations for the Project Team to use with the Care team to prepare them for implementation. These presentations and other helpful resources can be found on the MQii Tools & Resources page:
| Implementation Tool | Clinical Workflow Stage |
| Recognizing Malnutrition: A visual guide for diagnosis and assessment | • Malnutrition Screening • Assessment & Diagnosis |
| Sample Validated Screening Tool: The Malnutrition Screening Tools | • Malnutrition Screening |
| Nutrition Focused Physical Exam * Nutrition Focused Physical Exam Mini-Session webinar recording available to MQii Learning Collaborative participating organizations | • Assessment & Diagnosis |
| Nutrition Care Process Tutorial Videos | • Assessment, Diagnosis, Intervention, & Monitoring and Evaluation |
Additional online resources to help educate your Care team members on key aspects of malnutrition care include:
Once the Care team has been educated on the importance of malnutrition and how it can affect patient outcomes, and how to implement the clinical improvement activities, the Care team can then begin implementing the targeted changes to your clinical workflow. Please refer to the MQii Tools & Resources for additional materials to help support your MQii implementation efforts.
Please note that not all sites may focus on clinician education and training for their quality improvement activities. For example, some may choose to change how data is captured in the EHR to improve documentation and care coordination. Others may include “hard stops” or reminders in the EHR to ensure certain steps in the recommended clinical workflow take place. These actions are also important mechanisms to ensure the provision of high-quality care and meet the goals of quality improvement- focused changes.
Proper documentation of nutrition care is critical to support high quality data collection and to assess changes that take place as a result of your quality improvement activities. It also benefits the patient, as it helps enable effective care coordination within the hospital as well as transitions when the patient leaves the hospital. All nutrition data collected should be recorded in the patient’s medical record (electronic medical records or paper medical records, as applicable) and use a standardized data collection template or process, where possible and appropriate.
You should aim to regularly collect data and evaluate your progress throughout implementation, as well as assess whether your change is maintained following implementation. For example, assuming an implementation timeline of 3 to 6 months, you may wish to collect data and evaluate your change following the first one or two months of implementation to see whether you have made progress, or if additional education, training, or other changes to support your quality improvement activities are necessary.
The MQii suggested quality measures and indicators inform the type and level of data you will need. To see needed data elements and calculation instructions for the eCQMs, see the Specification Manual; to see the data elements and calculation instructions for the indicators, see the MQii Data Management Guide. These resources provide a description of all of denominator and numerator criteria and a description of how to use each of the variables gathered for calculating performance rates. All of these resources are available at www.MQii.today in the MQii Tools & Resources section.
If a specific activity has been attempted for 3 months without any success or sign of improvement, it may be an opportunity to reassess the implementation approach or identify a different root cause that would be more beneficial to address. As implementation of selected activities are tested, there should also be consideration for suggested best practices for patient engagement, staffing, and care coordination.
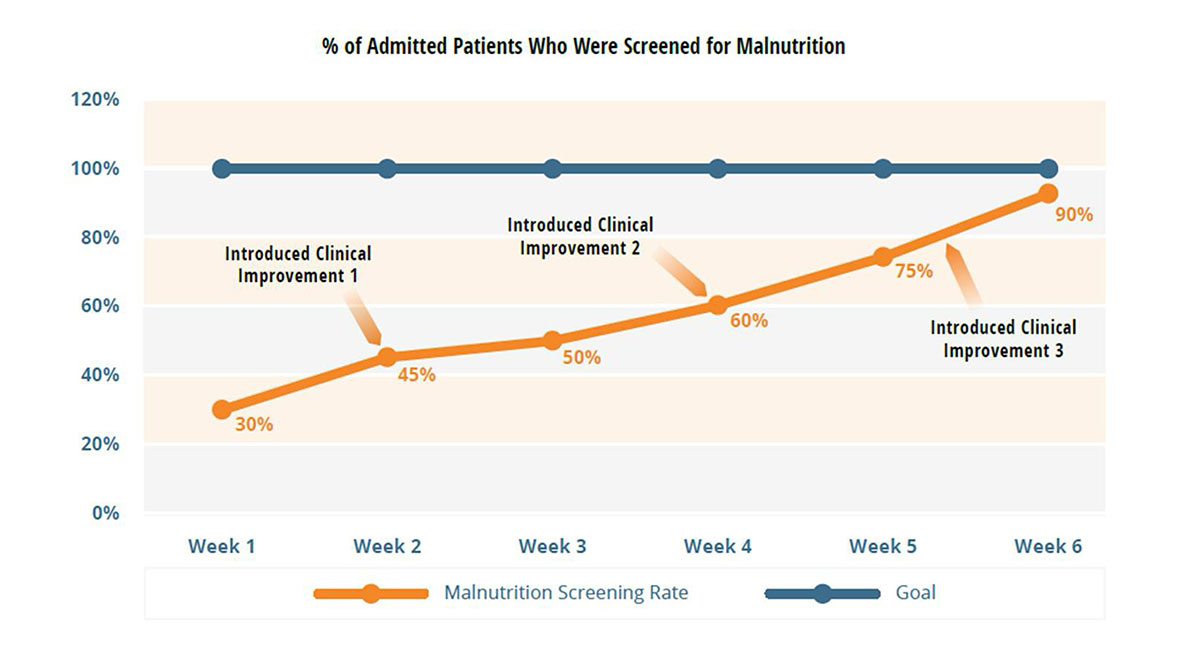
Results from data collected on the quality measures/indicators should be interpreted by the Care team on a continuous basis to inform further improvements in the clinical workflow. Displaying the data graphically (e.g., using run charts) makes it easy to discuss the process of care and to pinpoint specific events and tie change, or lack of change, in the measurement over time as it relates to clinical improvement activities.
Below, a sample run chart displays data that suggest the targeted quality improvement – increasing rates of malnutrition screening – has been very successful towards a stated goal of 100%. The record also shows the point in time where specific clinical improvements were performed to permit the Care team to make decisions around the effectiveness of the selected clinical improvements in creating or sustaining improvement. The Care team is able to track progress on a weekly basis and determine that the changes introduced have been effective.
To ensure a level of validity to your findings (i.e., confirm that the results represent what is really taking place), you may wish to follow a set of signal rules.[45] Signal detection rules are used to show that the changes that are identified in a chart are non-random. Most of the rules require at least 6 and as many as 12 data points on either side of the median to be considered a signal.[45]
Run charts also enable comparison of performance against a specific standard and may help the Care team identify problem areas. In the second sample chart below, the same team has seen an overall increase in the number of eligible patients who receive a nutrition assessment. However, the assessments are not being completed within their desired time frame of 24-hours. By comparing the two charts, the team may choose to explore the reasons why, despite higher screening rates, the nutrition assessments are not completed in a timely fashion. The Care team should review data as a group to gain these types of insights and work on problems and potential solutions together. By having the Project and Care teams collaborate on interpretation, you will ensure that perspectives of the different Care team members are included in the problem-solving process.
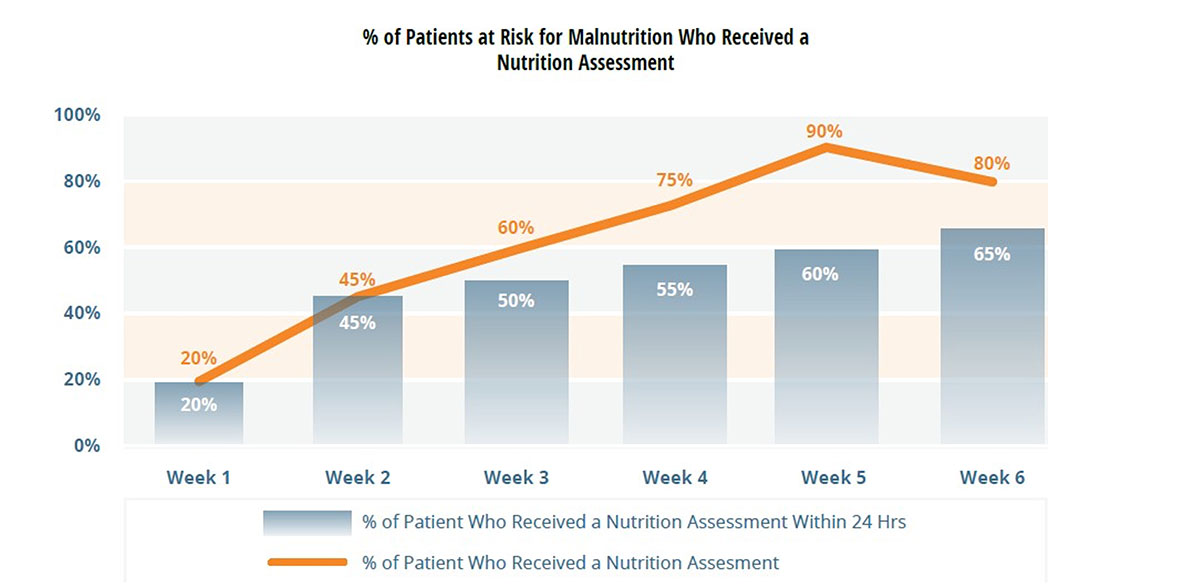
The Care team can use these results to identify specific aspects of the care process that might be adjusted to help bring about the desired outcome. It can be something as simple as a reminder pop-up on an intake assessment to additional training for the intake and transport staff. Ideally, the changes should be individual and incremental to be able to isolate and measure the effect of the change. Once the change is shown to be beneficial, that act of improvement should be shared with the broader Care team.
On this page:
MQii Toolkit:
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |

Members Area