Malnutrition Care Score for IQR
The Malnutrition Care Score quality measure is available for 2025 hospital reporting.
The Malnutrition Care Score quality measure is available for 2025 hospital reporting.
For individuals or teams with less familiarity with or direct experience implementing clinical quality improvement initiatives, it may be beneficial to review introductory quality improvement resources:
Prior to implementing the MQii at your hospital, be sure that there is institutional support and resources allocated to implement the initiative. Institutional support—from your executive staff, administrative staff, and clinician leaders—is essential for ensuring effective implementation. Key talking points and evidence supporting the need for QI are available on the MQii website.
To prepare for your initiative you will need to identify a Project Lead. This person leads day-to-day efforts for this initiative, including developing project management processes, spreading enthusiasm across the hospital for this project, and spearheading project implementation.
To continue building internal support and to understand your current state, you need to collect baseline data to demonstrate the need for improvement as well as to later use as a comparison when measuring your progress.
The key component of your baseline data is the existing malnutrition care workflow. Understanding your hospital’s current nutrition care workflow will enable the project team to identify differences between the existing clinical workflow and the recommended clinical workflow. This will help determine which stages of the clinical workflow have the most opportunity for improvement and what type of clinical improvement(s) or activities to introduce.
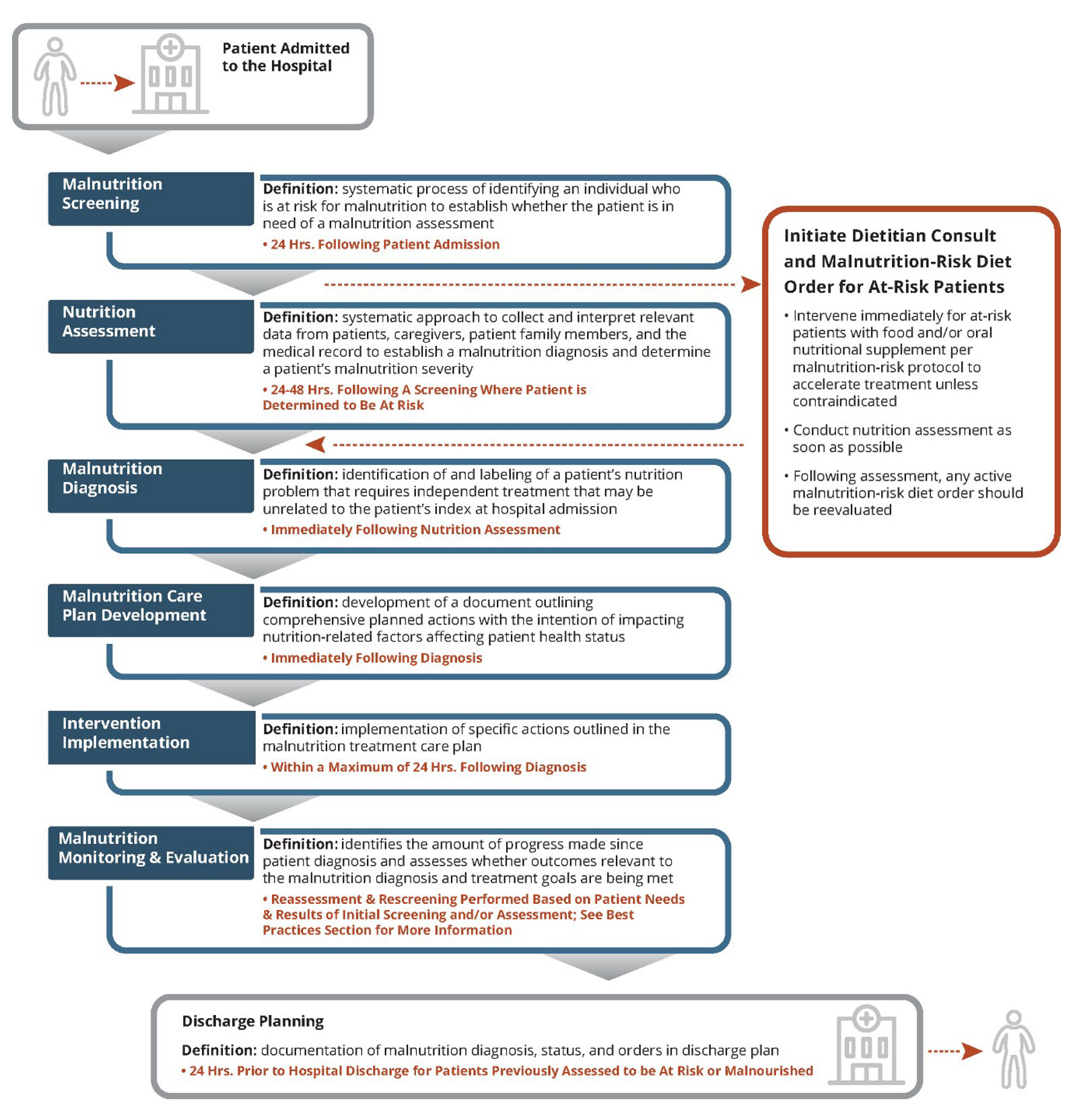
To assess your current clinical workflow for malnutrition care, we suggest mapping it using a process flowchart format. At a minimum, your flowchart should capture the process, timing, care team members involved, and documentation/hand off processes for each of the following steps of the malnutrition clinical care process:
Once completed, you can compare your flowchart to the recommended flowchart to evaluate how your current practices align with evidence-based standards. The figure below outlines the recommended process for nutrition care, including providing a definition of each of the steps outlined above and highlighting how each of these steps, including timing considerations, can fit together in your facility.
To further assist in selecting your quality improvement project, complete the Assessment and Decision Tool.
This resource asks a series of questions regarding your current care provision across each of the steps highlighted above to help your project team recognize where care is not aligned with best practices and opportunities for improvement exist.
Finally, quantify the gap between your current process and ideal state. For example, if you have collected data to evaluate the quality of your current clinical care provision using the Global Malnutrition Composite Score – you can review the findings from that data analysis to determine where your performance may be lower than you expected or hoped. If you don’t have access to pre-built reports from your hospital’s EHR, you can also do a simple chart review on a small randomly selected sample of patient charts, tracking “Yes” or “No” if each step of the malnutrition care process is documented in your sample charts. Your hospital’s Quality department may be able to help you in setting up baseline data collection and in conducting a chart review in accordance with HIPAA and applicable privacy policies. Once you have collected your baseline data, identify the steps in the malnutrition care process where you are consistently performing below a certain percentage (e.g., 90%) on screening, assessment, care plan development, etc. or if your timing is below recommended averages – these may suggest areas to target for quality improvement.
With a project lead and executive commitment in place for the initiative, the next step is to establish a well-defined, interdisciplinary MQii Project Team. The MQii Project Team is an interdisciplinary team that brings different perspectives to what is often a cross-functional problem and helps promote effective resource use.
Your facility can employ a degree of customization with the roles and assigned individuals for the project team, as needs vary by organization depending on the existing organizational structure. Your team may decide that not all project team roles are necessary, or an individual may take on more than one role.
It is strongly recommended that a physician champion be identified early on to help garner buy-in from leadership. If available at your facility, you may also consider representation from a patient advisory council to provide a patient perspective. That said, customize your project to the staff and resources that are needed and available.
Note that these are estimates, and the actual time commitment may vary.
Recommended Individual
Senior executive hospital leader (e.g., Chief Medical Officer, Chief Quality Officer).
Responsibilities
Hospital leader to champion the effort from a leadership perspective, and works to maintain executive leadership buy-in. A representative from the hospital’s C-Suite is highly recommended.
Estimated Time
~1 hour per month to review progress and approach.
Recommended Individual
Team leaders (i.e., clinical (RDN) leader and assigned representative from the hospital’s quality department).
Responsibilities
Leads day-to-day efforts for this initiative. Develops project management processes and spreads enthusiasm across the hospital for this project. Leads project implementation (e.g., leads clinician training). This role may be filled by the dietician champion together with the Quality team member.
Estimated Time
10 – 15 hours per month (depends on QI focus and resources).
Recommended Individual
Dietitian.
Responsibilities
If the project lead is not a dietitian, we recommend securing buy-in from a dietitian leader (CNM or Director) who will champion this effort in the nutrition department and make sure targeted QI changes are adopted. If the project lead is a dietitian, this role would overlap.
Estimated Time
4 – 6 hours per month (Depends on QI focus) or refer to project lead if dietitian is project champion.
Recommended Individual
Staff Nurse or Nurse Manager from a unit that admits patients.
Responsibilities
Nurses are the first line of defense to identify malnourished patients. They also play a critical role in implementing interventions and discharge planning. Having a nurse champion involved can facilitate training and education of nursing staff to make sure their nutrition care responsibilities are implemented effectively.
Estimated Time
3 – 4 hours per month (Depends on QI focus).
Recommended Individual
Physician.
Responsibilities
Clinician who generates support and buy-in for the project by all relevant parties and can communicate to other physicians in the hospital. Steps in when needed to move the project forward. Physician champion should meet at least monthly with the project lead to provide input and update communication to physicians.
Estimated Time
2 – 3 hours per month.
Recommended Individual
Informatics team member/ Data analytics representative.
Responsibilities
Assists with extraction of data elements required for GMCS or other metrics to assess compliance with the nutrition care process, length-of-stay, readmissions, as well as any other necessary data.
Estimated Time
40 hours total on average.
Recommended Individual
Individual from the hospital’s Patient and Family Advisory Council (if available).
Responsibilities
Although this may take slightly different forms across different health systems, the role of the patient voice is pivotal to the success of quality improvement. A patient’s perspective may add essential insights about their experiences within the healthcare system that can inform the direction of a particular project.
Estimated Time
Dependent on frequency of project team or steering committee meetings.
The care team consists of those responsible for direct patient care within the units implementing the initiative.
Roles & Responsibilities
Once the MQii project team has been established, the project manager should convene a kick-off meeting. This meeting will be used to:
In addition to clearly assigning and communicating the roles and responsibilities to all team members, project timelines should also be firmly established. To facilitate timely implementation and review of performance toward MQii goals, the project manager (or supporting team member) should schedule regular team meetings.
On this page:
MQii Toolkit:
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |

Members Area